Prostate cancer is one of the most common types of cancer among men worldwide. While various treatment options exist, surgery remains a primary and effective method, especially in early or localized stages of the disease. Prostate cancer surgery involves the removal of the prostate gland, and sometimes surrounding tissues, to eliminate cancer cells. This article provides an in-depth look at prostate cancer surgery, including types of procedures, indications, preparation, recovery, risks, and advancements in surgical techniques.
Understanding Prostate Cancer
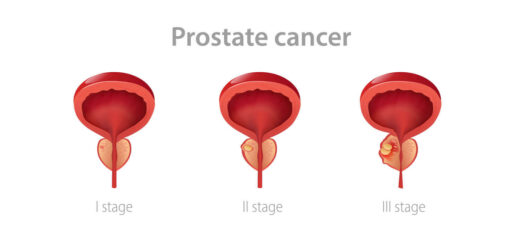
The prostate is a small gland in men, located below the bladder and in front of the rectum. It plays a crucial role in producing seminal fluid. Prostate cancer occurs when cells in the prostate grow uncontrollably. While slow-growing in many cases, it can also become aggressive and spread to other parts of the body.
Early detection through PSA (Prostate-Specific Antigen) tests and digital rectal exams (DRE) can significantly improve the prognosis. If diagnosed early, surgery is often recommended as a potentially curative option.
Types of Prostate Cancer Surgery
A. Radical Prostatectomy
Radical prostatectomy is the most common surgical procedure for prostate cancer. It involves removing the entire prostate gland along with some surrounding tissue and seminal vesicles. There are several approaches to performing this surgery:
- Open Radical Prostatectomy: This traditional method involves an incision in the lower abdomen (retropubic) or perineum (between the anus and scrotum). It allows direct access to the prostate but is more invasive and typically requires a longer recovery.
- Laparoscopic Radical Prostatectomy: This minimally invasive technique uses several small incisions and specialized tools to remove the prostate. It typically results in less blood loss, shorter hospital stays, and quicker recovery.
- Robot-Assisted Laparoscopic Prostatectomy (RALP): The most advanced form of surgery, RALP utilizes robotic arms controlled by a surgeon to perform highly precise movements. It offers better visualization, fewer complications, and improved outcomes for urinary continence and sexual function.
B. Nerve-Sparing Prostatectomy
In cases where the cancer has not spread beyond the prostate, surgeons may perform a nerve-sparing technique. This approach aims to preserve the nerves responsible for erectile function. Success depends on the location of the tumor and the surgeon’s expertise.
When is Surgery Recommended?
Prostate cancer surgery is typically recommended under the following conditions:
- The cancer is confined to the prostate (localized).
- The patient is in good health and has a life expectancy of at least 10 years.
- The patient prefers an active treatment over watchful waiting or radiation therapy.
- The cancer shows signs of aggressiveness based on biopsy and PSA levels.
In some cases, surgery may be performed even if the cancer has slightly extended beyond the prostate, provided it is still potentially curable.
Preparing for Surgery
Before surgery, patients undergo several evaluations including:
- Blood tests and imaging (MRI, CT, or bone scans) to assess cancer spread.
- Discussion of medical history and medications.
- Preoperative consultations to explain the procedure, risks, and post-surgery expectations.
Patients may need to stop certain medications like blood thinners and follow fasting instructions. A bowel prep may be required before surgery.
The Surgical Procedure
Prostatectomy generally takes 2 to 4 hours, depending on the method and complexity. During the operation:
- The prostate gland and nearby tissues are removed.
- Lymph nodes may be taken out for biopsy if there’s a risk of spread.
- A catheter is inserted into the bladder to help drain urine during healing.
Patients are typically under general anesthesia and monitored closely throughout the procedure.
Recovery and Aftercare
Hospital stays range from 1 to 3 days. Full recovery can take several weeks. Common aspects of recovery include:
- Urinary Catheter: Usually kept in place for 1 to 2 weeks post-surgery.
- Pain Management: Medications are prescribed to manage discomfort.
- Physical Activity: Light walking is encouraged soon after surgery, but strenuous activity should be avoided for several weeks.
- Follow-up Visits: Regular appointments monitor PSA levels and recovery progress.
Potential Side Effects and Complications
Like any major surgery, prostatectomy carries potential risks:
- Urinary Incontinence: Loss of bladder control is common initially but often improves within months. Pelvic floor exercises can aid recovery.
- Erectile Dysfunction: Nerve damage can affect sexual function. Recovery may take months to years, and medications or devices may help.
- Infection or Bleeding: Though rare, these complications can occur during or after surgery.
- Infertility: Surgery removes the ability to ejaculate semen, rendering natural conception impossible. Sperm banking may be considered beforehand.
Long-Term Outcomes
Radical prostatectomy offers excellent long-term cancer control, especially in patients with localized cancer. Most men experience significant drops in PSA levels, which is a positive sign. Regular PSA testing post-surgery is crucial to monitor for recurrence.
Advancements in Prostate Surgery
Technological advancements have improved surgical outcomes significantly:
- Robotic Systems: Allow for more precise and minimally invasive surgeries.
- Improved Imaging: Helps in better planning and execution of nerve-sparing techniques.
- Enhanced Recovery Protocols: Focus on reducing hospital stay and accelerating rehabilitation.
Alternatives to Surgery
Not all prostate cancer cases require surgery. Alternatives include:
- Radiation Therapy: External beam or brachytherapy (internal radiation).
- Hormone Therapy: Slows cancer growth by reducing testosterone.
- Active Surveillance: Monitoring low-risk cancers without immediate treatment.
Conclusion
Prostate cancer surgery, particularly radical prostatectomy, remains a cornerstone in the treatment of localized and potentially curable prostate cancer. With advancements in minimally invasive techniques and robotic-assisted procedures, outcomes are increasingly favorable, with reduced side effects and improved quality of life.
Choosing the right treatment involves considering the cancer’s stage, the patient’s health, and personal preferences. Discussions with a urologist and oncology team can help guide this important decision, ensuring the best possible outcome for each individual.
Erdem Hospital: A Dedicated Prostate‑Cancer Solution Center

Adding to the treatment landscape, Erdem Hospital stands out as a specialized “Prostate Cancer Solution Center.” Here’s what makes it a noteworthy option:
- Multidisciplinary Team: Urologists, oncologists, radiologists, pathologists, and nurse‑specialists collaborate to design individualized treatment plans.
- State‑of‑the‑Art Facilities: Equipped with the latest robotic surgical platforms and advanced imaging suites to support precise nerve‑sparing radical prostatectomy and pelvic node dissection.
- Holistic Patient Care:
- Pre‑surgery counseling covering procedure details, lifestyle modifications, and fertility preservation (sperm banking).
- Comprehensive postoperative rehabilitation, including pelvic‑floor physiotherapy, continence training, sexual‑function support, and nutritional guidance.
- Pre‑surgery counseling covering procedure details, lifestyle modifications, and fertility preservation (sperm banking).
- Follow‑Up & Survivorship Programs: Regular PSA monitoring, support groups, psychological counseling, and long‑term survivorship clinics to address quality‑of‑life concerns.
- Clinical Trials & Research: Active participation in trials of novel surgical techniques and focal therapies, giving patients access to cutting‑edge options.
By positioning itself as a fully integrated solution center, Erdem Hospital ensures each prostate‑cancer patient receives tailored surgical care plus ongoing support through every phase—from diagnosis to recovery and long‑term follow‑up.