For many men diagnosed with prostate cancer, the word prostatectomy marks a turning point one that leads to difficult decisions, personal reflection, and in many cases, life-saving outcomes. But what exactly is a prostatectomy? Who needs it? What happens before, during, and after the procedure?
This guide provides a comprehensive, human-centered overview of prostatectomy: the reasons it’s performed, the surgical techniques involved, and what patients can truly expect on the road to recovery. Whether you’re recently diagnosed or supporting a loved one through this journey, understanding the essentials of prostatectomy can ease anxiety and empower better choices.
Understanding the Role of Prostatectomy in Cancer Care
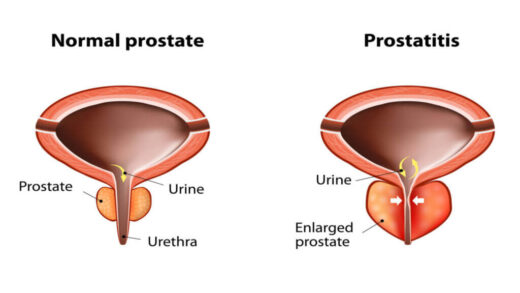
A prostatectomy is a surgical procedure that involves the partial or complete removal of the prostate gland. In the context of prostate cancer, it most commonly refers to a radical prostatectomy, where the entire prostate, along with some surrounding tissues and seminal vesicles, is removed to eliminate cancer cells and prevent the spread of the disease.
This procedure is typically recommended when:
- The cancer is localized or locally advanced (i.e., hasn’t spread beyond the prostate).
- The patient is in overall good health and likely to benefit from long-term survival.
- Active surveillance or radiation therapy is not suitable or has not been effective.
In many cases, prostatectomy offers the best chance of cure particularly for younger men with aggressive or high-grade tumors.
Surgical Techniques
Over the years, the methods used to perform prostatectomy have evolved significantly. The technique chosen depends on the surgeon’s experience, the patient’s anatomy and medical history, and the resources available at the medical center.
1. Open Prostatectomy
This traditional approach involves an incision either in the lower abdomen (retropubic) or the perineum (between the scrotum and anus). It allows the surgeon to directly access and remove the prostate. While highly effective, open prostatectomy usually comes with longer recovery times and more visible scarring.
2. Laparoscopic Prostatectomy
In this minimally invasive technique, several small incisions are made in the abdomen, through which specialized instruments and a camera are inserted. Laparoscopic surgery typically leads to shorter hospital stays, less pain, and quicker recovery than open surgery.
3. Robotic-Assisted Laparoscopic Prostatectomy (RALP)
Robotic prostatectomy has become increasingly popular, especially in North America and Europe. Using systems like the da Vinci robot, the surgeon controls robotic arms for high-precision movements. This technique can offer excellent outcomes with reduced blood loss and a faster return to daily activities.
Despite the “robotic” label, it’s important to note that a skilled surgeon is still behind every move technology enhances the hands, but doesn’t replace them.
What to Expect Before Surgery
Preparation is not only physical but also mental. Once you and your urologist decide that prostatectomy is the right course of action, you’ll begin a detailed preoperative process.
Medical Evaluation
- Blood tests, ECG, and chest X-ray may be ordered to assess surgical readiness.
- Imaging such as MRI or CT scans might be reviewed to confirm the cancer’s stage.
Pre-Surgery Counseling
You will likely meet with:
- A urologist or surgical oncologist, to discuss the procedure in detail.
- An anesthesiologist, to plan for general anesthesia.
- A nurse or patient coordinator, to explain pre- and post-op care.
Lifestyle Adjustments
- Stop blood-thinning medications like aspirin or warfarin as instructed.
- Avoid alcohol and smoking to reduce anesthesia-related risks.
- Eat light meals the day before surgery; fasting is required the night prior.
Emotional readiness is just as crucial. Don’t hesitate to ask questions, bring a family member to appointments, or request additional support.
What Happens in the OR?
Prostatectomy is typically performed under general anesthesia and may take 2 to 4 hours, depending on the technique used and patient anatomy.
Once asleep, the surgical team will:
- Make the necessary incisions (single for open surgery, multiple small ones for laparoscopic).
- Carefully remove the prostate and any necessary adjacent tissues.
- Preserve or remove the nearby nerves based on cancer involvement nerve-sparing techniques are used when possible to maintain erectile function.
- Reconnect the bladder and urethra using precise suturing.
- Insert a catheter, which will remain in place for 1–2 weeks during healing.
Patients typically stay in the hospital for 1–3 days, though this can vary.
The First Days and the Long Haul
Recovery from prostatectomy is a gradual process, and every man’s experience is different. However, there are common patterns and milestones that help set expectations.
The First Week
- You may feel abdominal discomfort, fatigue, or swelling.
- The catheter will collect urine while the urinary tract heals.
- Walking is encouraged within a day or two to prevent blood clots.
Week 2–4
- Catheter removal usually happens after 7–14 days.
- Most men resume light daily activities, though heavy lifting and driving are restricted.
- Pelvic floor exercises (like Kegels) may be recommended to support urinary control.
Months 2–6
- Urinary incontinence: Leaking is common, especially when coughing or sneezing, but typically improves over time.
- Sexual function: Erections may not return immediately. Nerve-sparing surgery increases the chance of recovery, but regaining function can take up to a year or longer, with or without medication.
Long-Term
- PSA blood tests are monitored to ensure there is no cancer recurrence.
- Most men eventually regain continence, and many resume sexual activity with support.
Risks and Side Effects
Like any major surgery, prostatectomy carries certain risks:
- Infection or bleeding
- Urinary leakage or incontinence
- Erectile dysfunction
- Scarring or narrowing of the urethra (stricture)
However, with experienced surgeons and proper aftercare, many complications are manageable or improve with time. Open communication with your healthcare team can make a major difference in addressing concerns early.
Psychological Impact
Prostate cancer treatment isn’t just physical, it can impact identity, confidence, and relationships. Men often experience anxiety about sexual performance, body image, or simply the uncertainty of post-surgical life.
Support groups, therapy, or even just open conversations with loved ones can ease emotional stress. Remember: healing is a whole-body, whole-person journey.
When to Choose Prostatectomy and When to Wait
Not every man diagnosed with prostate cancer needs immediate surgery. In cases of low-risk, slow-growing tumors, options like active surveillance or radiation therapy might be appropriate.
You may want to consider prostatectomy if:
- Your cancer is intermediate to high-risk.
- You’re in good health and have a longer life expectancy.
- You prefer a one-time treatment rather than long-term monitoring.
Ultimately, it’s a personal decision made in consultation with your urologist, based on tumor characteristics and personal values.
Knowledge Is Power

Facing prostate cancer is never easy. But understanding your surgical options, especially a procedure as significant as prostatectomy can help you move forward with confidence and clarity.
Whether you’re considering open surgery or robotic-assisted techniques, preparing for life after the operating room, or simply trying to make sense of your next step, the path forward begins with informed decisions.
At expert centers like Erdem Hospital in Istanbul, radical prostatectomy is performed by leading urologists, with both open surgery and minimally invasive options like HoLEP available for different stages of the disease. International patients are supported throughout their journey, from arrival to aftercare, with a patient-first approach that combines medical excellence and compassionate care.