A torn anterior cruciate ligament (ACL) is one of the most feared injuries among active individuals and for good reason. Whether it happens during a misstep on the football field or an awkward landing in a pickup basketball game, an ACL tear can take away your stability, mobility, and confidence in a split second.
But thanks to remarkable advances in orthopedic medicine, a torn ACL doesn’t have to be the end of your active life. Modern ACL reconstruction surgery has evolved into a precise, minimally invasive procedure with excellent outcomes. In this article, we break down what happens when the ACL tears, how surgery works today, and why so many people are moving again stronger than ever after going under the knife.
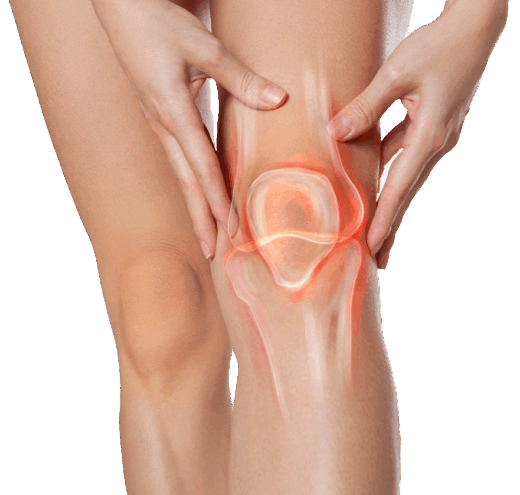
What Is the ACL, and Why Does It Matter?
The anterior cruciate ligament (ACL) is one of four main ligaments that stabilise the knee joint. It runs diagonally in the centre of the knee, connecting the femur (thigh bone) to the tibia (shin bone). Its primary functions are:
- Preventing the tibia from sliding too far forward
- Controlling knee rotation during pivoting and side-to-side motion
- Providing overall joint stability during motion
When the ACL is torn whether partially or completely the knee often becomes unstable. This instability can make everyday activities difficult and return to sport nearly impossible without intervention.
Common Causes of ACL Tears
ACL injuries often result from sudden movements such as:
- Pivoting or cutting (changing direction quickly)
- Sudden deceleration
- Awkward landings after a jump
- Direct blows to the knee (common in contact sports)
While athletes are at higher risk, ACL injuries can happen to anyone even during recreational activities or accidents. Women, in particular, face a higher risk due to anatomical and hormonal differences.
Symptoms of a Torn ACL
Most ACL injuries are acute and highly noticeable. Common signs include:
- A “popping” sound at the moment of injury
- Immediate pain and swelling
- Loss of range of motion
- A feeling that the knee is unstable or “giving way”
Left untreated, a torn ACL can increase the risk of further damage to the cartilage or meniscus, leading to chronic pain and even early arthritis.
Can a Torn ACL Heal Without Surgery?
This is one of the most frequently asked questions and the answer depends on the severity of the injury, the patient’s lifestyle, and the level of knee instability.
- Partial tears: In some cases, conservative treatment like physiotherapy and bracing can help.
- Complete tears: Especially in active individuals or those who require high knee function, surgical reconstruction is often the only way to regain full stability.
If your knee buckles during daily activities or prevents you from returning to sport or work, surgery is usually recommended.
Modern ACL Reconstruction Surgery: What’s Changed?
Over the last two decades, ACL reconstruction has seen major advancements in both surgical technique and post-operative outcomes. Here’s what modern ACL surgery looks like today:
1. Minimally Invasive Arthroscopy
Most ACL reconstructions are now performed using arthroscopic techniques. This involves:
- Small incisions
- A camera (arthroscope) inserted into the joint
- Precision tools for graft placement
This leads to less tissue trauma, reduced scarring, faster recovery, and lower infection risk.
2. Use of Grafts to Rebuild the Ligament
Since the ACL cannot be stitched back together, it must be reconstructed using a graft. Common graft options include:
- Autografts: Tissue from your own body (usually patellar tendon, hamstring, or quadriceps tendon)
- Allografts: Donor tissue from a cadaver (often used in older patients or revision surgeries)
Each graft has pros and cons, and your surgeon will select the most appropriate one based on your age, activity level, and goals.
3. Anatomic Graft Placement
Modern techniques focus on reproducing the ACL’s original anatomical footprint. This allows for more natural knee biomechanics, improving both function and long-term outcomes.
What to Expect During Recovery
While surgery is an important milestone, rehabilitation is just as crucial. A structured, supervised rehab plan is key to regaining strength, mobility, and confidence. The process generally includes:
Phase 1: Immediate Post-Op (Weeks 1–3)
- Pain and swelling management
- Range of motion exercises
- Walking with crutches
Phase 2: Strength and Stability (Weeks 4–12)
- Quadriceps and hamstring strengthening
- Stationary cycling and pool therapy
- Weight-bearing progression
Phase 3: Functional Training (Months 3–6)
- Balance and proprioception exercises
- Agility drills
- Light jogging
Phase 4: Return to Sport (6–12 Months)
- Sport-specific drills
- Psychological readiness assessment
- Final medical clearance
Return-to-sport timelines vary. On average, athletes resume competitive play within 9–12 months, but this depends on individual progress and surgeon recommendations.
Success Rates and Long-Term Outcomes
Modern ACL reconstruction has excellent outcomes, especially when performed by experienced orthopedic surgeons. Key statistics:
- 90%+ of patients report good to excellent function within one year post-op
- 70–85% of athletes return to their pre-injury level of sports
- Lower risk of future meniscal or cartilage injury compared to untreated ACL tears
It’s also important to follow neuromuscular training post-recovery to prevent re-injury, especially among young athletes.
Real Stories, Real Results
Athletes across the world have returned to peak performance after ACL surgery. While famous success stories often involve professional players, everyday individuals from weekend runners to fitness instructors also report life-changing results.
Take James, a 35-year-old amateur footballer in London, who tore his ACL during a local league match. After arthroscopic ACL reconstruction and 10 months of physiotherapy, he returned to competition with full mobility, no pain, and even improved sprint mechanics. Or Aisha, a 28-year-old yoga teacher from Manchester, who feared she’d never practice again. Today, she leads five classes a week after undergoing a successful hamstring graft reconstruction.
These aren’t exceptions. They’re the new standard, thanks to modern ACL techniques and disciplined rehabilitation.
Risks and Considerations
As with any surgical procedure, ACL reconstruction carries potential risks, including:
- Infection
- Blood clots
- Graft failure
- Joint stiffness
- Residual instability
However, complications are relatively rare, especially when patients follow post-operative guidelines and engage in proper rehabilitation.
It’s also worth noting that re-injury is possible, especially in younger athletes returning to high-risk sports. A preventive strength and movement training program is essential to reduce that risk.
When to Consider ACL Surgery
You may be a candidate for ACL reconstruction if you:
- Have a complete ACL tear
- Experience frequent instability or “giving way”
- Wish to return to sports or physically demanding work
- Are concerned about long-term joint damage
- Have failed conservative management (like physiotherapy)
Your orthopedic specialist will help guide the decision-making process, taking into account your goals, activity level, and overall knee health.
Don’t Let a Torn ACL Hold You Back
A torn ACL can feel like a devastating setback but it’s not the end of the road. Thanks to the evolution of surgical techniques, personalised rehabilitation, and better understanding of biomechanics, modern ACL reconstruction gives you a real chance at a full, confident return to motion.
Whether you’re a professional athlete, a weekend warrior, or simply someone who wants to walk, run, or play without pain, ACL surgery can help you get there.
Talk to an experienced orthopedic surgeon today to discuss your options and start your journey toward a stronger, more stable knee.