Benign Prostatic Hyperplasia (BPH) is a common condition that affects aging men, characterized by the non-cancerous enlargement of the prostate gland. This enlargement can lead to urinary symptoms and significantly impact the quality of life. While BPH is not life-threatening, its symptoms can be bothersome and may worsen if left untreated. Fortunately, a wide range of treatment options are available, from lifestyle changes and medications to minimally invasive therapies and surgical procedures.
In this article, we will explore everything you need to know about BPH treatment — including when to seek treatment, available options, and what to expect.
Understanding BPH
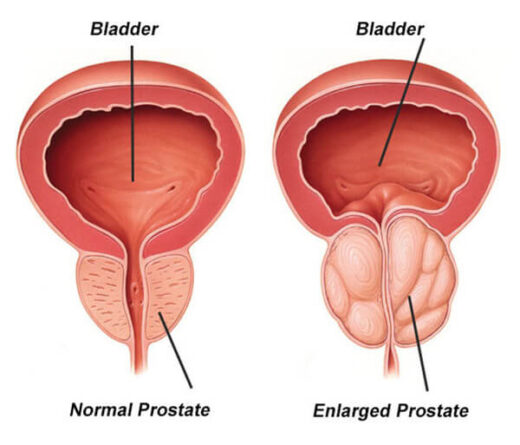
The prostate is a small gland located below the bladder and in front of the rectum. It surrounds the urethra — the tube that carries urine from the bladder out through the penis. As men age, the prostate tends to enlarge. This process is influenced by hormonal changes, particularly involving testosterone and dihydrotestosterone (DHT).
An enlarged prostate can compress the urethra, causing various urinary symptoms such as:
- Frequent urination, especially at night (nocturia)
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Feeling of incomplete bladder emptying
- Urgency to urinate
- Dribbling at the end of urination
While these symptoms are common, they can also indicate other conditions, such as urinary tract infections (UTIs) or prostate cancer, making proper diagnosis essential.
Diagnosis of BPH
Diagnosis of BPH begins with a thorough evaluation by a healthcare provider. This typically includes:
- Medical History and Symptom Review: The International Prostate Symptom Score (IPSS) questionnaire is often used to assess the severity of symptoms.
- Digital Rectal Exam (DRE): The doctor checks the size and shape of the prostate.
- Urinalysis: To rule out infections or blood in the urine.
- Prostate-Specific Antigen (PSA) Test: Elevated PSA levels can suggest prostate enlargement, but may also indicate prostate cancer.
- Urinary Flow Test: Measures the strength and amount of urine flow.
- Postvoid Residual Volume Test: Determines how much urine remains in the bladder after urination.
- Imaging Tests: Ultrasound or cystoscopy may be performed in certain cases.
Treatment Options for BPH
Treatment for BPH depends on the severity of symptoms, the size of the prostate, age, overall health, and patient preference. Management options fall into several categories:
1. Watchful Waiting (Active Surveillance)
Men with mild or non-bothersome symptoms may not need immediate treatment. Instead, they are monitored regularly through checkups to track symptom progression. Lifestyle changes are often recommended, including:
- Reducing caffeine and alcohol intake
- Limiting fluid intake in the evening
- Practicing bladder training techniques
- Avoiding medications that can worsen symptoms, such as decongestants or antihistamines
2. Medications
Medications are typically the first-line treatment for moderate to severe symptoms of BPH. Common drug classes include:
a. Alpha Blockers
These medications relax the muscles of the prostate and bladder neck, improving urine flow and reducing symptoms. They work quickly, often within days to weeks.
Common alpha blockers:
- Tamsulosin (Flomax)
- Alfuzosin (Uroxatral)
- Doxazosin (Cardura)
- Silodosin (Rapaflo)
Side effects may include dizziness, fatigue, or ejaculation problems.
b. 5-Alpha Reductase Inhibitors (5-ARIs)
These drugs shrink the prostate by blocking the hormone DHT, which contributes to prostate growth. They may take 3–6 months to show noticeable effects.
Common 5-ARIs:
- Finasteride (Proscar)
- Dutasteride (Avodart)
Side effects include decreased libido, erectile dysfunction, and reduced semen volume.
c. Combination Therapy
Sometimes, alpha blockers and 5-ARIs are used together for greater effectiveness, especially in men with significantly enlarged prostates.
d. Phosphodiesterase-5 Inhibitors
Tadalafil (Cialis), commonly used for erectile dysfunction, is also approved for treating BPH symptoms, particularly when ED and BPH coexist.
3. Minimally Invasive Treatments
For patients who do not respond well to medications or prefer to avoid surgery, minimally invasive procedures offer effective alternatives with quicker recovery times.
a. Transurethral Microwave Thermotherapy (TUMT)
This procedure uses microwave energy to heat and destroy excess prostate tissue. It is done on an outpatient basis.
b. Transurethral Needle Ablation (TUNA)
TUNA delivers low-level radiofrequency energy through needles inserted into the prostate. It’s a safe option for moderate symptoms.
c. Prostatic Urethral Lift (UroLift System)
UroLift involves the placement of tiny implants that lift and hold the enlarged prostate tissue away from the urethra, thus improving urine flow. It is performed under local anesthesia and has a low risk of sexual side effects.
d. Rezūm Water Vapor Therapy
Rezūm uses steam to destroy excess prostate tissue. It is a newer, minimally invasive option with promising results.
4. Surgical Treatments
Surgery is recommended for men with severe symptoms, complications such as urinary retention, recurrent UTIs, bladder stones, or when other treatments have failed.
a. Transurethral Resection of the Prostate (TURP)
TURP is the most common surgical procedure for BPH. It involves removing prostate tissue using a resectoscope inserted through the urethra. TURP is highly effective but requires hospital stay and catheterization for a few days.
b. Holmium Laser Enucleation of the Prostate (HoLEP)
HoLEP uses a laser to remove large amounts of prostate tissue. It is ideal for very large prostates and has a lower risk of bleeding.
c. Open or Robot-Assisted Prostatectomy
This is reserved for very large prostates. The surgeon makes an abdominal incision to remove prostate tissue. Recovery time is longer compared to minimally invasive options.
Managing Expectations and Follow-up
BPH treatment is typically very successful, especially when tailored to the individual. However, follow-up is essential to monitor for symptom recurrence, medication side effects, or new complications.
After surgical treatment, some men may experience temporary incontinence or retrograde ejaculation (semen entering the bladder during orgasm). These issues are typically manageable and improve over time.
Conclusion
BPH is a common and treatable condition affecting millions of men worldwide. With advances in medical therapies and minimally invasive techniques, most patients can achieve significant relief from symptoms without resorting to major surgery. Early diagnosis and open communication with a healthcare provider are essential for choosing the best treatment strategy.
Whether through lifestyle modifications, medication, or advanced procedures, men with BPH have many tools available to regain control over their urinary health and improve their quality of life.
Erdem Hospital: The Premier Choice for BPH Treatment

At Erdem Hospital, we combine cutting-edge technology, expert urologists, and patient-centered care to provide the most effective and personalized treatment for Benign Prostatic Hyperplasia (BPH). Whether you need advanced diagnostics, modern medication management, or minimally invasive surgical options like UroLift, HoLEP, or laser therapy, our team ensures you receive world-class care with minimal recovery time.
With decades of experience and a commitment to excellence, Erdem Hospital is your trusted partner for restoring comfort, control, and confidence in your urinary health.