Ozempic has quickly become a buzzword in both the diabetes community and the wider world of weight loss. Social media is filled with success stories of people shedding pounds and seeing their blood sugar drop, all thanks to this injectable medication. But like most trends in medicine, the reality is far more nuanced. Behind the glossy headlines are growing reports of side effects, some mild, others serious enough to make both doctors and patients reconsider long‑term use.
At the same time, another solution for type 2 diabetes has been quietly proving itself for decades: gastric sleeve surgery. Far from being just a “weight‑loss operation,” this procedure is increasingly being recognized as a powerful tool for putting type 2 diabetes into remission. The question is, for many people living with diabetes, which option makes more sense in the long run?

The Promise of Ozempic
Ozempic, known generically as semaglutide, was developed to help people with type 2 diabetes lower their blood sugar levels. It works by mimicking GLP‑1, a hormone that helps the body release insulin, slows down digestion, and reduces appetite.
The benefits were clear from the start. Patients not only saw their HbA1c levels improve, they also started losing weight, sometimes a significant amount. In a world where type 2 diabetes and obesity so often go hand in hand, this dual effect was game‑changing.
But medications that act on the body so powerfully often come with trade‑offs.
What We’re Learning About Side Effects
Like many medications, Ozempic has its share of predictable, common side effects. Nausea, vomiting, diarrhea, and constipation are so typical that doctors warn patients to expect them, especially in the first few weeks. For most, these settle down. For some, they don’t and the constant nausea becomes a reason to quit.
More concerning are the less common, but potentially serious complications that have surfaced as the drug’s popularity has exploded.
- Digestive emergencies: Reports have linked GLP‑1 drugs like Ozempic to tens of thousands of ER visits in the U.S. for severe vomiting, abdominal pain, and bowel blockages.
- Vision problems: A recent study in Israel suggested a two‑fold increase in risk for a serious retinal condition called neovascular age‑related macular degeneration (nAMD) in Ozempic users. Other reports have raised questions about sudden vision changes and even optic nerve damage.
- Thyroid concerns: Animal studies found an association with certain thyroid tumors, which led to an FDA warning. People with a family history of medullary thyroid cancer are told to avoid the drug entirely.
- Mental health risks: Researchers are exploring possible links between GLP‑1 drugs and higher rates of depression, anxiety, and even suicidal thoughts. While rare, the possibility is enough that European regulators are actively reviewing the data.
- Loss of muscle and bone: Rapid weight loss from Ozempic isn’t just fat it can be up to 40% lean muscle mass, especially in older adults or anyone not doing strength training. That’s a hidden side effect that can weaken the body long‑term.
Even cosmetic side effects have made headlines: “Ozempic face,” the term for sudden facial sagging as subcutaneous fat melts away.
None of these findings erase the fact that Ozempic helps many people. But they do complicate the idea of taking it indefinitely, which is often necessary because weight regain is common when the injections stop.
Gastric Sleeve Surgery
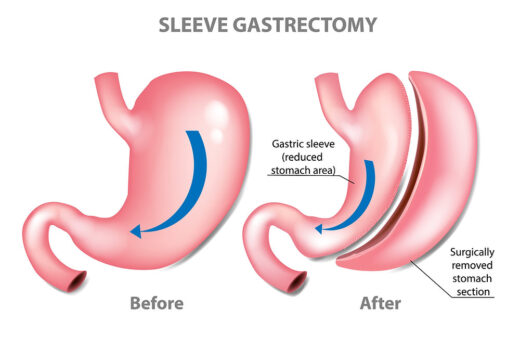
If Ozempic is the newcomer on the scene, gastric sleeve surgery is the seasoned veteran. In this procedure, about 75–80% of the stomach is removed, leaving a narrow “sleeve.” The result isn’t just a smaller stomach, it’s a major hormonal shift. Levels of ghrelin, the hunger hormone, drop sharply, appetite shrinks, and the body’s insulin sensitivity improves almost immediately.
The impact on type 2 diabetes can be remarkable. Studies consistently show that up to 85–90% of patients experience full or partial remission. Many leave the hospital already needing less medication or none at all.
And unlike drugs that must be taken week after week, the effects of gastric sleeve are long‑lasting. Weight loss is usually significant (often 50–70% of excess body weight within two years) and the metabolic reset can endure for decades.
Risks: The Honest Comparison
No treatment is without risk, and surgery is no exception. Gastric sleeve surgery can lead to leaks, infections, or bleeding in rare cases. Patients must commit to lifelong vitamin supplementation to avoid deficiencies in B12, iron, and calcium.
But when we step back and compare:
- Ozempic requires indefinite use to keep weight off and blood sugar stable, with ongoing exposure to its side effect profile.
- Surgery involves a single, up‑front intervention with a brief period of surgical risk but decades of potential benefit.
It’s also worth noting that serious complications from sleeve gastrectomy are uncommon (less than 5%), and mortality is extremely low (around 0.01%).
Who Should Consider Which?
For someone with mild obesity, newly diagnosed type 2 diabetes, and fear of surgery, Ozempic may be a sensible place to start with close medical monitoring.
But for someone with a BMI over 35, long‑standing diabetes, and growing medication needs, gastric sleeve surgery can be transformative. It doesn’t just lower blood sugar; it often removes the need for diabetes medication altogether.
Why More Doctors Are Steering Patients Toward Surgery
An eye‑opening study compared weight loss from GLP‑1 drugs with bariatric surgery. After two years:
- People on Ozempic lost about 5% of their body weight.
- People who had sleeve gastrectomy lost about 24% five times more.
And here’s the key for diabetes: the more weight lost, the more likely diabetes is to go into remission.
Doctors are also increasingly aware that weight cycling, losing and regaining weight, as often happens when stopping GLP‑1 therapy can be harmful in itself. Surgery offers a more permanent metabolic reset.
Lifestyle, Not Just Medicine

Neither Ozempic nor gastric sleeve is a magic bullet. Both require changes in how you live and eat.
- For Ozempic: maintaining muscle mass through strength training, eating enough protein, and staying under medical supervision are critical.
- For surgery: patients must stick to new eating habits, take vitamins, and keep up with follow‑up appointments.
The difference is durability. Stop taking Ozempic, and the weight usually creeps back. Stop following a perfect diet after gastric sleeve, and weight regain is possible too but the metabolic effects of the surgery mean it’s much easier to maintain weight loss.
So, Which Path Is Best?
There’s no one‑size‑fits‑all answer. Ozempic is a lifeline for people who aren’t ready or able to undergo surgery, or who need an interim tool to manage blood sugar and weight. Gastric sleeve surgery is a more aggressive intervention but one that often brings a permanent solution for those living with type 2 diabetes.
The real takeaway? This isn’t a contest between a drug and a surgery. It’s about finding the right tool for the right patient and being honest about the risks and rewards of each.
For many, that conversation is the first step toward not just lower blood sugar, but a life free of the constant fight with weight and worsening diabetes.